What is it?
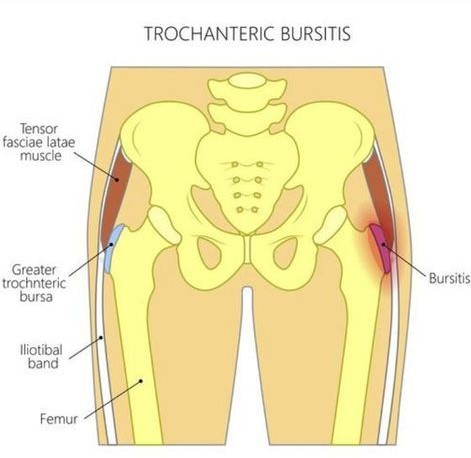
Bursa are small, fluid-filled sacs that lie between tendon and bone. They are all around the body and their main role is to reduce friction between the two structures. In hip bursitis the two structures are the femur (thigh bone) and the iliotibial band (ITB).
Bursitis is an inflammation of a bursa.
Here is bursitis in the hip:
What causes the bursa to become inflamed?
Commonly, there is a recent change in activity as well.
E.g. increase in exercise levels, change from a sedentary to an active job.
What does hip bursitis feel like?
Pain tends to be localised to the side of the hip. Initially the pain might be sharp. Over time it may radiate further around the hip and groin becoming more dull. It will be worse with repetitive moving of the leg or higher impact activity e.g. jump, run, or even just walking. It will likely increase in intensity over time, unless the causative factors are addressed.
Other symptoms include redness, swelling, warmth, tenderness to touch the area.
How do I know if it is hip bursitis?
If your symptoms fit the above explanation, and respond to anti-inflammatory measures then it is a likely diagnosis. This could include reduction of strain on the area (changing the way you sit/stand/move and reducing aggravating activities), ice, medication (check with GP if you are unsure whether you can take anti-inflammatories).
There are many other structures in the hip, lower back and pelvis that could be causing your pain and therefore an assessment from a healthcare professional can be helpful to confirm the diagnosis.
It is also important to rule out infection or inflammatory conditions such as Osteoarthritis or Rheumatoid Arthritis. Normally with these, your symptoms will be more constant rather than vary in intensity depending what you are doing. If you have any concerns, contact your doctor.
What can Back In Action Physio do?
The goal of treatment is to offload the affected bursa to reduce inflammation. We can help achieve this through use of taping, orthotics, muscle release, back or pelvis treatment, advice around how to modify your daily activity. As it improves, it is important that the return to normal tasks, work, and exercise is gradual to reduce the likelihood of symptoms returning. Your physio will guide you through a progressive rehab program that’s appropriate for you and your goals.