What Is It?
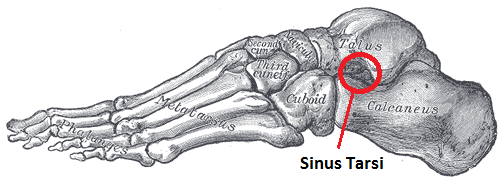
Sinus tarsi syndrome is pain or injury to the area (the tunnel) between the talus and the calcaneus bones. It is characterised by pain at the anterolateral side of the ankle (the outside of the foot below the ankle). Pain is worse when standing, walking on uneven ground or during ankle movements of the foot. People suffering from sinus tarsi syndrome can also have a feeling of instability (functional instability) in the hind foot. Symptoms of sinus tarsi syndrome tend to come on gradually over time.
How dose it happen?
Traumatic injury to the ankle such as an ankle sprain, or overuse such as repetitive standing or walking, are the main causes of this syndrome. It may also occur if the person has a pes planus or an over-pronated foot, which can cause compression in the sinus tarsi. When the syndrome is a result of an inverted ankle sprain there is a greater chance that the lateral collateral ligaments of the ankle are also damaged, since the ligaments in the sinus tarsi are the last ones to tear with a traumatic ankle sprain.
Reduced stability in the ankle will allow a greater range of motion to the subtalar joint. This excessive movement can increase forces onto the synovium and across the sinus tarsi. It is the subtalar joint synovitis which is responsible for chronic inflammation and infiltration of fibrotic tissues in the sinus tarsi and results in ankle pain. Injuries can also damage ligaments of the tibiotalar and talocalcaneal joints and increase the mobility between the talocrural and subtalar joints.
Sinus tarsi syndrome mainly occurs after a traumatic lateral ankle sprain or multiple ankle sprains (mostly due to a weak anterior talofibular ligament) which leads to injuries of the interosseus and cervical ligaments. The ligaments of the sinus tarsi can be sprained or torn and inflammation of the synovial recess in the sinus tarsi can occur and usually happens in 70% of cases. This pathology is mostly a result of synovitis and infiltration of fibrotic tissue into the sinus tarsi space due to an instability of the subtalar joint, caused by ligamentous injuries. When sinus tarsi syndrome occurs when people have flat or pronated feet, it is due to the talus and calcaneus being closer together and as a result can cause inflammation in the sinus.
What dose it feel like?
• Pain: tends to be localised to the sinus tarsi area, feels deep inside and gets worse with prolonged activities such as walking or running and eases with rest.
• Instability: especially when exercising on uneven ground or slopes, when jumping or quickly changing direction.
• Stiffness: the ankle may feel stiff first thing in the morning and then improve as you move around.
• Tender to touch: around the outside and front of the ankle.
• Pain with ankle movements: especially inversion (turning the sole of the foot inwards) and plantarflexion (pointing the foot down).
How is it diagnosed?
A full Physiotherapist assessment is the best way to diagnose Sinus Tarsi Syndrome. An MRI may be needed if symptoms are not settling which may show synovitis in the tunnel area.
What should I do if I have Sinus Tarsi Syndrome?
RICE: Rest is important for recovery in the initial stages and avoiding the aggravating activities to help efficient healing. Ice and NSAID’s (anti-inflammatory medication) can help to reduce pain and swelling in the area.
Footwear: Supportive footwear to prevent excess subtalar joint motion to stabilise the foot.
What can Back in in Action do to help?
Taping or strapping: Used to limit movement in the ankle and foot and reduce symptoms.
Insoles: These may be prescribed to limit motion at the subtalar joint and reduce symptoms, orthotics can also address biomechanics to prevent further occurrence.
Proprioception exercises: Single leg standing for 30 seconds, ten times per day, on either foot, will challenge the body’s response to an altered base of support. Eyes closed will make this harder as balance is affected by the lack of sight, therefore the body is challenged further to maintain upright stance.
Range of movement exercises: Active motion of the foot and ankle to improve restricted range.
Joint mobilisations: If there is ankle stiffness mobilisations can help release structures which cause poor range of motion.
Strengthening exercises: Long term rehab to strengthen the muscles around the ankle, which includes the peroneal muscles on the outside of the ankle, the gastrocnemius and soleus which make the calf muscles and the tibialis posterior muscle on the inside of the ankle.